Lyme Disease

Lyme disease is an infectious disease caused by the bacterium Borrelia burgdorferi, a spirochete (spy-ro–keet) that is transmitted to humans through the bit of infected black-legged (or deer) ticks and western black-legged ticks. It is the most common tick-borne illness in the United States.
An infected tick can transmit the spirochete to humans. The transmission of Borrelia burgdorferi typically occurs after the tick has been attached to a human for at least 36-48 hours because the bacteria reside in the tick gut and it takes time to migrate to the salivary glands.
The percentage of tick bites that result in Lyme disease varies based on several factors, including the type of tick, the duration of attachment, the tick’s infection status, and the region or locality. However, current data suggest that between 1 and 5% of tick bites actually result in successful infection with B. burgdorferi and resultant Lyme disease.
Several factors contribute to this:

Tick’s Infection Status: Not every blacklegged tick is infected with the Borrelia burgdorferi bacterium that causes Lyme disease. The percentage of ticks infected varies by region. In some areas, only a small fraction of ticks might be infected, while in others, more than 50% might carry the bacterium.
Duration of Attachment: Ticks generally need to be attached for at least 24 hours (some sources suggest 36-48 hours) to transmit the Lyme bacterium. This is because the bacterium requires time to migrate from the tick’s gut to its salivary glands. Ticks detected and removed promptly are less likely to transmit the disease.
Geographic Region: In areas endemic for Lyme disease, such as parts of the northeastern, north-central, and Pacific coastal U.S., the risk of encountering infected ticks is higher. However, even in these areas, the likelihood of an individual tick bite leading to Lyme disease isn’t 100%.
Estimates: In some Lyme-endemic areas, estimates suggest that the risk of developing Lyme disease after a recognized deer tick bite, if the tick is not removed promptly, might be around 1-3%. However, this figure can vary depending on the specific circumstances and factors mentioned above.
Remember, the best protection against Lyme disease is preventing tick bites in the first place. If bitten, prompt removal of the tick and monitoring for symptoms is crucial. If any symptoms arise, or if there’s uncertainty about the type and duration of the tick attachment, consulting with a healthcare professional is essential.
Untreated, the bacteria may travel from the site of the tick bite via the bloodstream, and can cause a number of symptoms, some of which may be severe. Often, an erythema migrans (EM) rash appears within 7-14 days at the site of a tick bite (click to see picture of a typical EM rash). Lyme disease manifests as a multisystem inflammatory disease that affects the skin in its early, localized stage, and can potentially spread to the joints, nervous system and, less commonly, other organ systems in later, disseminated stages.
If diagnosed and treated early with antibiotics, Lyme disease is almost always readily cured. Even in later stages, Lyme disease can also be treated effectively, but because the rate of disease progression and individual response to treatment varies from one patient to the next, some patients may have symptoms that remain for months or even years following treatment. In rare instances, Lyme disease may cause permanent damage.
Although Lyme disease is the most common arthropod-borne illness in the U.S., diagnosis and treatment can be challenging for clinicians due to its diverse manifestations, similarity of symptoms to other medical conditions, and the limitations of currently available serological (blood) tests. The prevalence of LD in the northeast and upper mid-west is due to the presence of large numbers of the deer tick’s preferred hosts – white-footed mice and deer – and their proximity to humans.
Ticks become infected with Borrelia burgdorferi by feeding on animals that serve as a reservoir for the bacteria. In North America, these are primarily white-footed mice, but other small rodents such as voles and chipmunks, as well as bird species can serve as reservoirs. These “reservoirs of infection” are fed on by larval and nymphal (juvenile) ticks which thereby become infected with the Lyme disease bacteria. An infected tick can then transmit infection the next time it feeds on another host (e.g., an unsuspecting human).
While deer are the preferred host for adult black-legged ticks, they are not a good reservoir, as bacteria do not seem to be transmitted efficiently in deer. Raccoons, opossums, and squirrels may serve as incidental hosts for the bacterium, but they are less effective as reservoirs as well.
Humans are a “dead-end” or incidental host for both ticks and Borrelia burgdoferi.
Early Localized Lyme Disease
- Erythema migrans (EM) rash
- Occurs in approximately 60 to 80 percent of infected persons
- Begins at the site of a tick bite after a delay of 3 to 30 days (typically 7-14 days)
- A tick bite at that skin site, however, is only recalled/noticed by ~25% of patients with a single EM skin lesion in the US
- Is typically a red and annular shaped skin rash that is at least 2 inches in diameter
- Expands gradually over several days reaching up to 12 inches or more (30 cm) in diameter
- May feel warm to the touch but is rarely very itchy or very painful
- Sometimes partially clears as it enlarges, resulting in a target or “bull’s-eye” appearance
- May appear on any area of the body
The “Bulls-Eye” Rash or Erythema Migrans (EM) is one of the classic symptoms of early localized Lyme disease. EM is not always a distinctive bulls-eye – sometimes it is more uniform in appearance, or faint in color – particularly in folks with darker skin. It’s also important to note that not all EM like rashes are a result of Lyme disease, so the circumstances surrounding a rash are always important for diagnosis. Swollen lymph nodes (lymphadenopathy) may occur near the site of the EM rash.
- Fever, chills, headache, fatigue, and/or muscle and joint aches may occur in early Lyme disease in patients with EM, but can also occur from B. burgdorferi infection in the absence of EM.

Lyme Arthritis

Neurologic Lyme Disease
Cranial nerve symptoms: facial nerve weakness (facial palsy/drooping), which can occur asymmetrically or symmetrically.
Peripheral nerve involvement: radiculoneuropathy which can cause numbness, tingling, “shooting” pain, or weakness in the arms or legs.
Central nervous system symptoms: Lyme meningitis (inflammation of the meninges) with fever, headache, sensitivity to light, and stiff neck.

Lyme Carditis
Lyme Carditis (occurs days to months after tick bite):
Lyme carditis can occur when B. burgdorferi spreads to the heart tissue, which can interfere with normal heart function. Lyme carditis, however, occurs in fewer than 1% of Lyme disease cases.
Lyme carditis can cause light-headedness, fainting, shortness of breath, heart palpitations, or chest pain.
Carditis can interfere with the normal beating of the heart, leading to “heart block,” which can vary in degree. While Lyme carditis can potentially be fatal, that is extremely rare. There have been 11 cases of fatal Lyme carditis reported globally over a period of 34 years (1985-2019).




How do we diagnose Lyme disease?
The diagnosis of early Lyme disease presenting with EM (erythema migrans) is clinical. The characteristic skin lesion present at the site of an Ixodes scapularis tick bite in individuals living in Lyme endemic regions is diagnostic.
Laboratory diagnosis is recommended in patients suspected of having Lyme disease from Lyme endemic areas presenting with atypical skin lesions, disseminated disease such as multiple skin lesions, neurological (meningitis, facial nerve palsy) or cardiac (myocarditis, atrio-ventricular block) symptoms, as well as those with arthritis that develops few weeks or months after the infection.
Since Lyme disease is caused by a bacterium (Borrelia burgdorferi) that is difficult to culture and is present in low numbers in clinical samples during early stages of infection, the main modality of laboratory confirmation is the detection of antibodies to the microorganism (Serology).
The current guidelines for antibody testing include the use of a 2-step testing. The first step uses an antibody assay such as an Enzyme Immunoassay (EIA) that has high sensitivity to detect IgG and IgM antibodies to B. burgdorferi (Bb); if this first step test is positive, it is followed by a second step EIA that will confirm the first step. The second step can use IgG and IgM western blots (WB) or immunoblots (IB) (Standard two-tier testing, STTT), or another EIA that uses different antigens than the first step (Modified two-tier testing, MTTT). The STTT uses IB interpretation criteria for IgG and IgM that had been previously evaluated and published. The IgM IB criteria uses 3 blot bands (41, 39 and 23-kDa, OspC) and the IgG IB criteria uses 10 bands (93, 66, 58, 45, 41, 39 30 28 and 23 and 18-kDa). In order to fulfill the IgM criteria, 2 of those 3 bands need to be detected and 5 of those 10 bands for IgG IB. Since these guidelines were adopted at the Second conference on Lyme diagnostics in Dearborn MI, and the Centers for Disease Control was one of the sponsors, it became known as the “CDC criteria”. Besides the bands to be scored, the guidelines established that the IgM IB criteria is only to be used during the first 4 weeks of early disease, but the IgG at any stage of the disease. The advantage of the MTTT is that IB, that suffer from interpretation limitations, are not used in addition to eliminating the 4-week IgM blot restriction. The two-step testing has limited sensitivity during early disease with EM (25 – 50% in acute sample to about 70% in convalescent phase sample) but increases to over 70 % to 100% in samples from patients with disseminated or extracutaneous manifestations of Lyme disease.
What are the limitations of current diagnostics?
The limitations are predominantly due to the complexity of B. burgdorferi (Bb) and those of serology.
The ideal laboratory method to support the diagnosis of an infectious disease is the direct detection of the organism causing disease, that in Lyme disease is difficult since Bb is not usually detected in clinical samples. Detecting antibodies is an indirect method that suffers limitations since it relies on the immune response of an infected individual to the antigens expressed by the infecting microorganism.
Regarding the complexity of Bb, this bacterium possesses most of the genes encoding its important antigens in plasmids, rather than in the chromosome. This allows Bb the plasticity to express antigens according to the environment that encounters. These antigens might differ when Bb is in a tick midgut or in the tissues of an infected mammal. As Bb is transmitted by a tick to a human, the antigens expressed by the microorganism stimulate the immune system leading to the development of antibodies that can vary depending on the patient’s immune response, the microorganism pathogenic characteristics, the antigens expressed and the duration of disease.
But the complexity of Bb goes beyond geographic boundaries. Bb causing infections in different geographic locations in the northern hemisphere are heterogeneous leading to different clinical manifestations. There are over 20 genospecies within Bb, being B. burgdorferi sensu stricto (Bbss), the most frequent causing infection in North America. B. afzellii and B. garinii along with Bbss cause Lyme disease in Europe. While all genospecies cause LD with EM, they differ in the later manifestations that they cause.
In addition to the antigenic complexities and geographic variations, antibodies to microorganisms appear within weeks, therefore they might not be detectable during early stages of the infection. That is the reason why serology works better when acute and convalescent phase samples are tested. If diagnostic antibodies are not present during the acute phase, they might be during the convalescence. Serology is not the recommended test when patient presents with a classical EM but might be useful in later disease stages as indicated above.
Other limitations of serology for Lyme disease include the persistence of detectable antibodies even after the disease has successfully been treated; therefore, serology is not recommended to follow the effect of treatment. In addition, the presence of antibodies as detected by these tests does not confer protection and these antibodies do not correlate with disease activity.
What are the current updates on new Lyme diagnostics?
Most current advances in Lyme diagnostics have dealt with searching and identifying antigens that could be used in more sophisticated assays, such as multiplex antibody assays using flow cytometry or on a chip. Other methods such as metabolomics or proteomics looking at signature biomarkers are being evaluated but as of now, they are not ready for diagnostic use.
What are ways Lyme cannot be diagnosed?
Tests that have not been appropriately validated should not be used to diagnose Lyme disease. These include tests offered by commercial laboratories such that offers culture enhanced PCR, FISH (fluorescence in-situ hybridization), CD57 detection, T lymphocyte response, or western blots employing their own interpretation criteria. In addition, culture offered by commercial laboratories should not be used for the diagnosis of Lyme disease. Use of microscopy for diagnosis is not accurate or approved. Use of PCR in blood, CSF, urine or other body fluids are of very low yield and should not be used. Exception to this is PCR of synovial fluid that can be helpful in untreated patients with Lyme arthritis.
Examples of Commericial Laboratories offering non-standard Lyme tests:
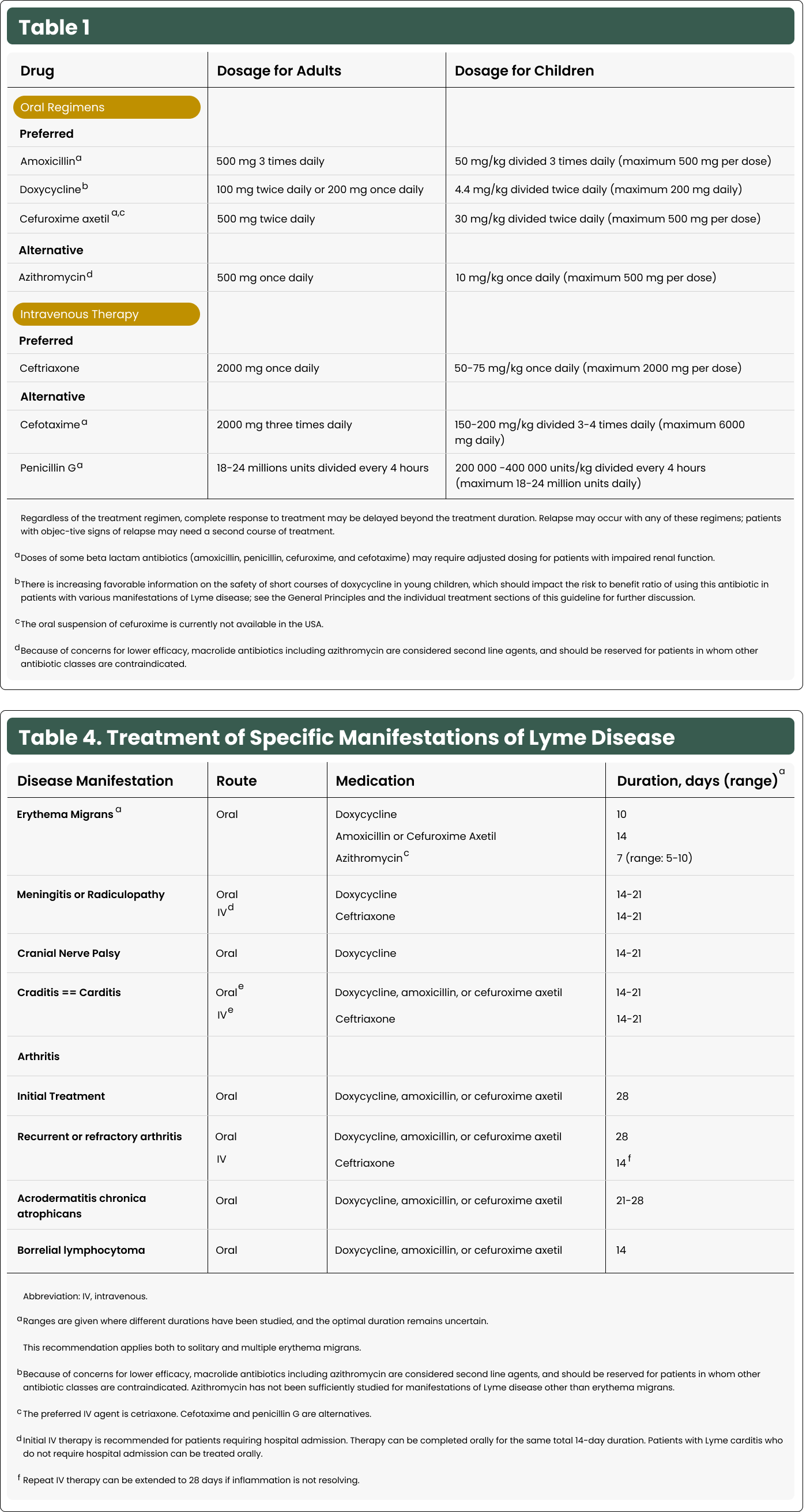
All treatments approved and supported by available evidence are the use of antibiotics to clear this bacterial infection. Lyme disease, regardless of whether it remains localized at the site of the tick bite or is one of the 10-20% of infections that has disseminated to another body site, is caused by a bacterial infection. As such, antibiotics, which are chemicals that kill bacteria, are typically successfully used. Treatments are standardized and reviewed periodically by reputable organizations such as the CDC, the Infectious Diseases Society of America (IDSA) and others. There are 3 main oral antibiotics that are prescribed for Lyme infections. Dosage depends on age and duration on the clinical presentation. If you have contraindications to these 3: doxycycline, amoxicillin, and cefuroxime, there are second-line antibiotics that can be used.


More often, though, chronic Lyme disease is used as a diagnosis to refer to a chronic and persistent case of Lyme disease, where people are believed to be continually infected with Borrelia burgdorferi. Some practitioners and members of the public use the term “chronic Lyme disease” to describe a scenario where they believe that the Borrelia burgdorferi infection persists despite treatment, causing ongoing symptoms. This perspective contends that the bacteria can evade the immune system and antibiotic therapy, leading to a chronic infection. However, this concept is not accepted by credible infectious disease experts and among the broader medical community because it lacks robust scientific evidence. Reputable medical authorities, including the CDC and IDSA (Infectious Diseases Society of America), do not recognize “chronic Lyme disease” in this context due to the lack of scientific proof of persistent infection.
It’s important to distinguish between these two usages because they imply different approaches to treatment. PTLDS is managed with supportive therapies aimed at alleviating symptoms, whereas the notion of “chronic Lyme disease” as an ongoing infection has led some to pursue prolonged antibiotic treatments and other unsubstantiated treatments, which are not supported by current evidence and can be harmful.
Most often you will find “chronic Lyme disease” being used by practitioners outside mainstream medicine (or medical providers without training in infectious diseases) to attribute a wide array of non-specific symptoms to an ongoing infection with Borrelia burgdorferi. However, unlike with PTLDS, this group of individuals never had an objective manifestation of Lyme disease and never tested positive for Borrelia burgdorferi infection by reputable laboratories.
What is Post-treatment Lyme Disease Syndrome (PTLDS)?
Lyme disease, an acute bacterial infection caused by Borrelia burgdorferi transmitted by Ixodes ticks, has been the center of controversy for decades. Post-Treatment Lyme Disease Syndrome (PTLDS) is a term used to describe a subset of Lyme disease patients who continue to report subjective symptoms after receiving standard antibiotic treatment for Lyme disease. This observation has been documented since the 1990s and is not a new phenomenon.
PTLDS does not mean the bacteria are still present in the body. It refers to post-infection sequelae, a condition where symptoms can persist after an acute infection is eliminated. This can occur in response to a variety of infectious diseases, and in the case of Lyme disease, has been named PTLDS.
The exact causes of PTLDS are not fully understood. Current data suggest a few possible explanations for why symptoms persist among some people:
Immune System Response: After an infection, the immune system may continue to react as if the body is under attack, even when the bacteria are gone. This can lead to inflammation and symptoms like pain and fatigue.
Tissue Damage: The bacteria that cause Lyme disease might damage tissues and organs during the infection. Even after the bacteria are killed, the body may still need time to heal from this damage, and symptoms could continue until this healing is complete.
Autoimmune reaction: It’s possible that the immune system starts to mistakenly attack the body’s own cells, leading to autoimmune problems. This could be triggered by the initial infection and contribute to the ongoing symptoms.
Residual Effects of the Infection: Sometimes the symptoms are lingering effects of the infection on the body’s systems, such as the nervous system, and not necessarily an active infection.
It is estimated that approximately 10-20% of patients treated for Lyme disease may experience PTLDS. The actual number can vary based on specific population studies, on how Lyme disease and PTLDS are defined, and on the criteria used for diagnosis.
Diagnosis of PTLDS is one of exclusion and should also include the history of confirmed Lyme disease, prior receipt of recommended antibiotic treatment, and the presence of symptoms such as fatigue, cognitive symptoms, or musculoskeletal pain for at least six months after treatment. These symptoms should significantly impact daily functioning and not be attributable to other medical conditions. If persistent but do not impact functioning, they are instead referred as Post-Treatment Lyme Disease Symptoms. Because these symptoms are generic and present in a variety of other medical conditions that would be managed differently, a careful differential diagnosis is critical.
Research into PTLDS is ongoing, and studies are examining differences in immune responses among patients, trying to understand potential risk factors that may predispose someone to developing PTLDS, and more. Management of these symptoms involves supportive care; extended antibiotic treatment is not recommended.
How do I know if I’ve encountered chronic Lyme disease misinformation?
If the phrase chronic Lyme disease is not being used to refer to PTLDS, it inevitably is being used as a diagnosis referring to ongoing and persistent bacterial infection. There are several key phrases and language that will appear. Recognizing these can be a helpful red flag when assessing the credibility of the information.
Diagnostic red flags:
Doctor shopping, such as looking for doctors advertising non-standard diagnoses and treatments.
Implausible coinfections.
Use of unproven diagnostic tests, especially those sold over the counter, urine-based tests, using labs that promote non-standard tests, lab shopping (e.g., for those that report high rates of positive results), ignoring standard test results to diagnose Lyme anyway.
Treatment red flags:
Enormous amounts of prescriptions or OTC treatments
Expensive treatments (antibiotics cost $50 on average even without insurance)
Non-FDA approved treatments
Unproven treatments
Installation of PICC lines/IV treatments
Social red flags
Integrating into identity: “Lyme warrior”
Hostility toward evidence-based medicine and seeking naturopaths, functional medicine practitioners, or homeopaths
Talking about “biofilms,” “persisters,” or “cyst forms,” which are not real problems with Lyme disease
Someone who suffers from multiple dubious diagnoses, has family with them (Munchausen’s/Munchausen’s by Proxy, medical child abuse)
Joining Lyme advocacy organizations and ultimately becoming an advocate of these treatments


Lyme disease is an infectious disease caused by the bacterium Borrelia burgdorferi. In order to contract Lyme disease, you must be bitten by an infected black-legged tick or deer tick (Ixodes scapularis) in the northeastern and north-central United States or the western black-legged tick (Ixodes pacificus) on the Pacific Coast. Lyme disease can be transmitted by nymphal and adult ticks of these species, but not larval ticks. Nymphs are considered to be most responsible for transmitting Lyme disease to humans because of their small size, which makes them harder to detect. In order to transmit Lyme disease, the tick must be infected with the bacteria and must be attached and feeding for at least 24 hours in order to transmit the bacterium. The longer an infected tick is attached, the higher the likelihood it will transmit the bacteria.
Lyme disease is most commonly reported in the northeastern, north-central, and Pacific coastal regions of the United States. However, cases have been documented in nearly every state and also in many other countries. You are most likely to be exposed to ticks if you spend time in wooded or grassy areas where these tick species live. Activities like hiking, camping, or even gardening in endemic areas can increase the risk of coming into contact with an infected tick. It can take anywhere from 15 minutes to 2 hours for a tick to find a suitable place to attach after crawling onto you. After being outdoors, especially in areas where ticks are common, it’s crucial to check yourself, children, and pets thoroughly for ticks. This includes looking at hard-to-see areas like the armpits, groin, and scalp.
Lyme disease is not transmitted from person to person. For example, you can’t catch Lyme disease from touching, kissing, or having sex with a person who has Lyme disease. Lyme disease is not transmitted to humans from other biting vectors such as other tick species, mosquitoes, or fleas. While pets and wild animals can get infected with the bacteria that cause Lyme disease, it cannot be transmitted from animals to humans. However, pets can bring infected ticks into your home or yard, so it’s a good idea to check them regularly and use tick preventatives.
However, the characteristic skin rash known as erythema migrans (EM) presents in 60-80% of cases. It begins as a small red spot at the site of the tick bite and can expand over a period of days or weeks to form a large circular rash that often looks like a “bull’s-eye” with a clear center.
Other early symptoms are more generic and include fever, fatigue, headache, muscle and joint aches, and swollen lymph nodes. If these symptoms present along with epidemiologic evidence of a potential tick bite, your clinician may prescribe diagnostic testing for further confirmation. If you seek clinical evaluation with later symptoms of Lyme, these may present as joint pain and swelling, facial palsy, heart palpitations, dizziness, nerve pain, and neurological issues.
The following pathogens can also be transmitted by Ixodes scapularis and Ixodes pacificus ticks (the species that also transmit the Lyme disease bacteria Borrelia burgdorferi and Borrelia mayonii):
- Anaplasma phagocytophilum
- Ehrlichia muris eauclairensis
- Babesia microti
- Borrelia miyamotoi
- Powassan virus
Co-infections among individuals with evidence of early Lyme disease are uncommon: the best data suggests risk is less than 10%. Ecological surveillance of ticks in Lyme-endemic regions routinely reveals the presence of at least 2 microorganisms within sampled ticks. However, there is a difference between detection within ticks in the environment and the successful transmission and infection of multiple pathogens to a human.
Lyme disease, caused by the bacterium Borrelia burgdorferi and transmitted through the bite of infected ticks, presents with a variety of symptoms that can often overlap with those of other illnesses. This can sometimes make diagnosis challenging. While Lyme disease may be characterized by the hallmark “bull’s-eye” rash (erythema migrans), the remaining symptoms such as fatigue, joint pain, and neurological symptoms, can be present in a variety of other medical conditions.
- Rheumatoid Arthritis (RA): RA is an autoimmune disorder that affects the joints, causing pain and inflammation. Its symptoms, especially joint pain and swelling, can be mistaken for Lyme arthritis, a late-stage symptom of Lyme disease. Furthermore, both conditions can cause fatigue and generalized body aches.
- Fibromyalgia: This condition is characterized by widespread musculoskeletal pain, fatigue, and tenderness in localized areas. As with Lyme, patients with fibromyalgia might experience joint and muscle pain, severe fatigue, headaches, and difficulty sleeping.
- Chronic Fatigue Syndrome (CFS): Also known as myalgic encephalomyelitis, CFS presents with persistent and unexplained fatigue that doesn’t improve with rest. This profound fatigue, often accompanied by pain and cognitive difficulties, can mirror the symptoms of chronic Lyme disease.
- Multiple Sclerosis (MS): MS is a chronic autoimmune disease of the central nervous system. It can lead to muscle weakness, coordination and balance issues, and neurological symptoms. Some of these neurological symptoms, such as numbness, tingling, and visual disturbances, can also be seen in Lyme disease.
- Mononucleosis: Caused by the Epstein-Barr virus, mononucleosis presents with fatigue, sore throat, fever, and swollen lymph nodes. These symptoms can overlap with early presentations of Lyme disease.
- Systemic Lupus Erythematosus (SLE): Commonly known as lupus, SLE is an autoimmune disease that can cause fatigue, joint pain, rash, and fever, which are also symptomatic of Lyme disease.
- Bell’s Palsy: This condition involves the sudden weakness or paralysis of facial muscles, usually on one side of the face. Lyme disease can also cause facial palsy, which can make Bell’s palsy a differential diagnosis in Lyme-endemic areas.
- Depression: Fatigue, cognitive issues, sleep disturbances, and general feelings of malaise are common in depression. Given that these symptoms are also seen in Lyme disease, especially in its later stages, differentiation can be challenging.
- Anxiety Disorders: The neurocognitive and some physical symptoms of Lyme disease, such as tremors or palpitations, can be mistaken for manifestations of an anxiety disorder.
- Brain Fog and Cognitive Disorders: Difficulty concentrating, memory issues, and confusion, often referred to as “brain fog,” can be seen in conditions like Lyme disease and other disorders, such as depression, CFS, or even hormonal imbalances like hypothyroidism.
- Other Tick-borne Illnesses: Diseases like anaplasmosis, ehrlichiosis, and babesiosis are also transmitted by ticks and can have symptom overlap with Lyme disease. These are tick-borne illnesses caused by different bacteria but present with very similar symptoms to Lyme disease, including fever, fatigue, headache, muscle pain, and joint aches.
It’s essential to understand that the presence of one or more of the above symptoms does not automatically indicate Lyme disease. Misdiagnosis can lead to ineffective treatments and prolonged illness. Comprehensive medical evaluations, considering the patient’s complete medical history, potential exposure to ticks, and other diagnostic tests, are crucial. A differential diagnosis approach helps in ensuring that the actual underlying condition is identified and treated appropriately.
Diagnosing Lyme disease can be challenging because its signs and symptoms can mimic those of many other diseases. Diagnosis is based on a combination of clinical presentation, epidemiologic information, and diagnostic testing.
If, during clinical evaluation, the characteristic skin rash known as erythema migrans (EM) is noted, this is sufficient for diagnosis and commencement of antibiotic treatment. EM is a hallmark sign and appears in about 70-80% of infected individuals. It begins as a small red spot at the site of the tick bite and can expand over a period of days or weeks to form a large circular rash that often looks like a “bull’s-eye” with a clear center. Other early symptoms are more generic and include fever, fatigue, headache, muscle and joint aches, and swollen lymph nodes. If these symptoms present along with epidemiologic evidence of a potential tick bite, your clinician may prescribe diagnostic testing for further confirmation. If you seek clinical evaluation with later symptoms of Lyme, these may present as joint pain and swelling, facial palsy, heart palpitations, dizziness, nerve pain, and neurological issues.
Clinical symptoms should be weighed along with epidemiologic Information – the likelihood that a patient was potentially exposed to infected ticks. These factors that can support clinical suspicion include geographic location, prevalence of Lyme in that area, and recent time spent in wooded or grassy areas where Lyme disease is prevalent.
Diagnostic testing should include an FDA-approved two-tier testing method. Tests that claim to use non-standard methods or non-blood bodily fluids are not reliable and should not be used. These tests assess the immune response to the bacteria, and not the actual bacteria, so they cannot differentiate between a past infection and a current infection. Antibodies may be present in your blood years after prior Lyme infection.
Two-tier testing usually involves enzyme Immunoassay (EIA): This is the most commonly used initial screening test. If it is positive or equivocal, a Western blot test is usually performed next, although a secondary EIA may be performed instead following new CDC guidance. Western blotting detects antibodies against specific proteins of the Borrelia burgdorferi bacterium. Two types of Western blots are used for Lyme disease: IgM and IgG. A positive IgM response alone is not sufficient for diagnosis and can be misleading. Both IgM and IgG Western blots should be positive for a definitive diagnosis.
Additional Testing: For people with symptoms suggestive of neurologic or cardiac involvement, additional tests, like lumbar punctures or EKGs, may be ordered.
It’s essential to note the following:
- False positives: Tests can sometimes yield positive results even when a person doesn’t currently have Lyme disease (due to cross-reactivity with other infections or conditions and the fact that antibodies will be present after infection is no longer in the body).
- Timing matters: The body’s immune response can take several weeks to develop, so tests can be negative if done too soon after the tick bite.
Because of the limitations of current diagnostic testing, the diagnosis of Lyme disease should always be based on a combination of clinical presentation, history of exposure, and diagnostic testing. If you suspect you have Lyme disease or have been bitten by a tick, it’s essential to consult with a credible healthcare professional.
There is no credible scientific evidence to suggest that Lyme disease is sexually transmitted. The primary mode of transmission of the Borrelia burgdorferi bacterium, which causes Lyme disease, is through the bite of infected blacklegged ticks.
While Borrelia burgdorferi can be found in blood in some instances, it does not circulate in high numbers in the bloodstream, which means that it is not a blood-borne pathogen, a feature often necessary for sexual transmission of infectious agents. In addition, studies have not found viable Borrelia burgdorferi in human semen or vaginal secretions. Further, epidemiologic patterns of Lyme disease don’t correspond with sexually transmitted diseases. For example, there’s no increased risk of Lyme disease among sexually active people, unlike with genuine sexually transmitted infections.
Anecdotal reports about possible sexual transmission of Lyme disease are not supported by robust scientific studies.
There is no solid scientific evidence to suggest direct person-to-person transmission of Lyme disease under typical circumstances.
Blood Transfusions: While the bacterium can be found in the blood of infected individuals at low levels, transmission through blood transfusion has not been documented. As a precaution, people being actively treated for Lyme disease are often advised not to donate blood.
Pregnancy: Some concerns about the potential for transmission from an infected mother to her unborn child during pregnancy (vertical transmission). While there have been isolated reports of this happening, the evidence is not robust, and such transmission seems to be rare. Additionally, adverse outcomes in these cases are not consistently observed. Pregnant women who suspect they have Lyme disease should consult with their healthcare providers to evaluate the need for treatment.
Breastfeeding: There is no documented evidence of transmission of Lyme disease through breast milk. However, if a lactating mother has a Lyme rash (erythema migrans) on her breast, she should avoid breastfeeding from that side until she has received appropriate treatment.
Saliva and Casual Contact: There’s no evidence to suggest transmission of Lyme disease through saliva, kissing, or casual person-to-person contact.
No, getting bitten by a tick does not guarantee that you will contract Lyme disease. Several factors determine the risk:
Type of tick: Not all ticks carry the Lyme disease bacterium. In the United States, only blacklegged ticks (often referred to as deer ticks) in the Northeast, North Central states, and Pacific coast are primary vectors for Borrelia burgdorferi, the bacterium that causes Lyme disease.
Duration of attachment: The risk of transmission increases the longer the tick remains attached. Ticks that are removed within 24 hours are less likely to transmit Lyme disease. This is because the bacterium typically requires a longer time in the tick’s gut before it can migrate to the tick’s salivary glands and be transmitted to the host.
Tick’s infection status: Not every tick is infected with the Lyme disease bacterium. The percentage of ticks infected varies by region and local conditions. In some areas, only a small percentage of ticks might be carriers, while in other areas, more than half might be infected.
Prompt removal: Properly and promptly removing a tick reduces the risk of transmission. Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible. Pull upward with steady, even pressure. After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol, an iodine scrub, or soap and water.
Observation: After a tick bite, it’s essential to monitor for signs and symptoms of Lyme disease, which can appear within 3 to 30 days. The most common early symptom is a circular rash that looks like a bull’s-eye (erythema migrans), but not everyone with Lyme disease develops this rash. Flu-like symptoms such as fever, fatigue, headache, muscle and joint aches, and swollen lymph nodes may also occur.
If you experience symptoms of Lyme disease, it’s important to consult with a credible healthcare professional to determine next steps including appropriate antibiotic treatment if warranted.
Several factors contribute to this:
Type of Tick: Only certain tick species can transmit Lyme disease. In the United States, the blacklegged tick (or deer tick, Ixodes scapularis) in the Northeast, North Central states, and Pacific coast is the primary vector. On the West Coast, the western blacklegged tick (Ixodes pacificus) is responsible. Not all bites from these ticks will transmit Lyme disease.
Tick’s Infection Status: Not every blacklegged tick is infected with the Borrelia burgdorferi bacterium that causes Lyme disease. The percentage of ticks infected varies by region. In some areas, only a small fraction of ticks might be infected, while in others, more than 50% might carry the bacterium.
Duration of Attachment: Ticks generally need to be attached for at least 24 hours (some sources suggest 36-48 hours) to transmit the Lyme bacterium. This is because the bacterium requires time to migrate from the tick’s gut to its salivary glands. Ticks detected and removed promptly are less likely to transmit the disease.
Geographic Region: In areas endemic for Lyme disease, such as parts of the northeastern, north-central, and Pacific coastal U.S., the risk of encountering infected ticks is higher. However, even in these areas, the likelihood of an individual tick bite leading to Lyme disease isn’t 100%.
Estimates: In some Lyme-endemic areas, estimates suggest that the risk of developing Lyme disease after a recognized deer tick bite, if the tick is not removed promptly, might be around 1-3%. However, this figure can vary depending on the specific circumstances and factors mentioned above.
Remember, the best protection against Lyme disease is preventing tick bites in the first place. If bitten, prompt removal of the tick and monitoring for symptoms is crucial. If any symptoms arise, or if there’s uncertainty about the type and duration of the tick attachment, consulting with a healthcare professional is essential.
Lyme disease is caused by the bacterium Borrelia burgdorferi and is transmitted to humans through the bite of infected black-legged ticks. Once diagnosed, Lyme disease can usually be effectively treated with antibiotics, especially if the treatment starts early in the course of the disease, as is the case with other bacterial infections.
When Lyme disease is detected and treated with a standard course of oral antibiotics early, a full recovery is expected in the vast majority of cases. In some instances, if infection with certain strains of Borrelia burgdorferi are left untreated or if treatment is delayed, Lyme disease can progress to more advanced stages affecting the joints, heart, and nervous system. This can lead to more severe and prolonged symptoms. Even in these cases, treatment with antibiotics is still effective. However, recovery might be slower and some symptoms can persist.
In rare instances, some people continue to experience symptoms after successful completion of antibiotic treatment. This condition, often referred to as Post-treatment Lyme Disease Syndrome (PTLDS), can include fatigue, pain, or joint and muscle aches. The exact cause of PTLDS is not entirely understood, but it’s believed that the lingering symptoms may result from residual damage to tissues and inflammatory responses that occurred during the infection.
It’s important to note that there is no credible evidence that the bacterium persists in the body after treatment. Since Lyme disease refers to illness associated with bacterial infection, you are not considered to have Lyme disease following treatment. Successfully treating Lyme disease does not mean you are immune to future infections. This means that after recovery, it’s still possible to be bitten by another infected tick and contract Lyme disease again.
The specific type, dosage, and duration of antibiotic treatment depends on the clinical symptoms, but most often involve oral antibiotics for a duration of 10-28 days. In some instances, intravenous antibiotics may be administered for a period of time.
It is important to note that there are many treatments marketed for Lyme disease that are ineffective, unproven, and potentially harmful.
⚠️Treatments that are not recommended include:
Prolonged courses of antibiotics: Although antibiotics are the mainstay of treatment for Lyme disease, using them for extended periods (many months to years) has not been proven to be more effective than the recommended shorter courses. Moreover, prolonged antibiotic use can lead to dangerous side effects, opportunistic infections with other pathogens, and antibiotic resistance.
Alternative supplements or treatments: Various herbs, supplements, and other remedies might be promoted for treating Lyme disease, but there is limited scientific evidence supporting their effectiveness. Some examples include:
- Colloidal silver
- Hyperbaric oxygen
- Ozone
- Bee venom
- Detoxification diets
Heat or “thermotherapy”: The idea that exposing oneself to high temperatures (like in a sauna) can kill the Lyme-causing bacteria is not supported by evidence.
Avoiding mainstream medical care: Some people, frustrated by the symptoms or the challenges in diagnosis and treatment, might decide to bypass established medical practices altogether. This can be risky, especially when Lyme disease can have severe and long-term complications if not adequately treated.
Using treatments for “chronic Lyme disease”: This term is controversial and not widely accepted by the mainstream medical community. While post-treatment Lyme disease syndrome (PTLDS) is recognized, the term “chronic Lyme disease” often encompasses a wide array of symptoms without clear evidence of ongoing Borrelia burgdorferi infection. Some practitioners might offer unproven, longterm, and risky treatments based on this concept, which are not beneficial and can be harmful.
Estimates of the percentage of Lyme disease patients who go on to develop PTLDS vary based on the study and criteria used. It is estimated that 10% to 20% of patients who had legitimate Lyme disease may experience persistent symptoms after completing a standard course of antibiotics.
The exact cause of PTLDS is not fully understood. Current data suggest that it may result from the inflammatory response triggered by the infection or residual tissue damage that occurred during infection and not a persitent or ongoing infection with the bacterium Borrelia burgdorferi.
It’s important to note that while a percentage of Lyme disease patients may experience ongoing symptoms, the vast majority of these individuals will improve over a period of months, especially with appropriate management and supportive care. If someone believes they have PTLDS or is concerned about ongoing symptoms after Lyme disease treatment, they should consult with a healthcare professional.
The term “chronic Lyme disease” (CLD) is controversial and not universally recognized within the medical community. There are two primary contexts in which it’s discussed:
Post-Treatment Lyme Disease Syndrome (PTLDS): Some patients who are treated for Lyme disease continue to experience symptoms long after their treatment has finished. The more accepted term for this condition is Post-Treatment Lyme Disease Syndrome (PTLDS). Symptoms can include fatigue, joint or muscle aches, and cognitive dysfunction. The cause of PTLDS is not entirely understood, but it’s believed that the persistent symptoms are not due to ongoing infection with Borrelia burgdorferi. Instead, it’s theorized that PTLDS might result from an autoimmune response or residual tissue damage. The recommended treatment typically does not involve prolonged antibiotic therapy. In some contexts, people or healthcare providers may use the term ‘chronic Lyme disease’ in this context to refer to a collection of symptoms that remain after infection is eliminated with antibiotics, but does not refer to an ongoing or persistent infection.
“Chronic Lyme Disease” as a Diagnosis: Some practitioners and patients use the term “chronic Lyme disease” more broadly, referring to a variety of chronic symptoms in patients who may or may not have evidence of a prior Lyme disease infection. In many cases, these individuals have not met the clinical or epidemiological criteria for a Lyme disease diagnosis or may not have had documented evidence of a Borrelia burgdorferi infection. Many practitioners who diagnose this use unproven tests that report false positives using non-blood bodily fluids and unreliable testing technologies, leading people to believe they have an infection when they do not.
Some believe that these symptoms are due to a persistent, low-level infection with the bacterium and advocate for extended antibiotic therapy, often for months to years, in addition to other unproven treatments that have no evidence to support their use. However, several comprehensive studies have shown that long-term antibiotic therapy and these other treatments are not beneficial and can be harmful.
Remember, there are a variety of other medical conditions that have similar symptoms to the more generic signs of Lyme disease, and it is important to seek an accurate diagnosis from a credible healthcare provider.
It’s important to note that the symptoms associated with PTLDS or what some refer to as “chronic Lyme disease” are real and can be debilitating. The debate within the medical community is primarily around terminology, etiology (cause), and appropriate treatment.
If someone believes they have persistent symptoms associated with Lyme disease or any other unexplained health concerns, they should consult with a healthcare professional to discuss their symptoms, get a proper diagnosis, and explore treatment options.
Tick testing is generally unnecessary, and should not be a substitute for diagnosis by a physician. Just because a microorganism is found inside a tick does not mean the tick is capable of transmitting it to a human. Remember: tick physiology is vastly different from a human.
Tick testing is not always done in a clinical laboratory. Clinical labs have to adhere to high quality control standards that do not apply to non-clinical labs. As a result, results may not be accurate and should not guide treatment decisions.
Waiting for tick testing results to make treatment decisions can be risky, especially if symptoms develop before results are available.
Just as a positive test cannot tell you if you’ve actually been infected with a microorganism identified in a tick, a negative test can give false security, as it is possible another species of tick bit you and did transmit a pathogen.
You can send a tick in for testing if you want, but not doing so does not increase risk of illness. You should be aware of the limitations to the information gained from doing so.
- Ixodes scapularis (black-legged tick or deer tick) in North America:
- In the northeastern, north-central, and Pacific coastal regions of the U.S., studies have found that anywhere from 20% to 50% of nymphs (young ticks) carry the bacterium. Adult ticks can have slightly higher infection rates, sometimes exceeding 50% in certain areas.
- However, in the southeastern United States, the percentage of infected black-legged ticks is generally much lower.
- Ixodes pacificus (Western black-legged tick) in the Pacific Coast:
- This tick is less efficient than the deer tick at transmitting Lyme disease. In California, studies have generally found that less than 5% of these ticks carry Borrelia burgdorferi.
- Ticks in Europe:
- In Europe, the primary vector is Ixodes ricinus. The prevalence of Borrelia burgdorferi in these ticks varies significantly across regions, with reported rates ranging from under 10% to over 60% depending on the area.
- Other tick species:
- Several other tick species may have Borrelia burgdorferi in them, but they have not been demonstrated to be successful at transmitting the bacteria to humans.
It’s essential to remember that even if a tick is infected, transmission of the bacterium to humans is not guaranteed. The risk of transmission generally increases the longer the tick remains attached, with many sources suggesting a higher risk after 24 hours of attachment.
There was once a vaccine for Lyme disease, but it’s no longer available. The LYMErix vaccine was approved in 1998 by the U.S. Food and Drug Administration (FDA). This vaccine was developed to produce an immune response against the outer surface protein A (OspA) of Borrelia burgdorferi, the bacterium that causes Lyme disease. It was actually quite effective, demonstrating 76% efficacy at preventing Lyme disease in phase 3 clinical trials after a 3-dose vaccine regimen.
However, 1998 was the same year Andrew Wakefield’s falsified data came out in the Lancet that claimed MMR vaccines were linked to autism. This led to general mistrust of vaccines in general, and increased attention on any adverse events after any vaccination. Unfortunately this impacted the success of the Lyme disease vaccine.
After its release, vocal individuals raised concerns about the vaccine’s safety, suggesting it was causing arthritis. Public concern grew with increased media attention, even though these claims were unsubstantiated, there was no evidence of a causal relationship between vaccination and these reported adverse events, and rates of arthritis among vaccinated individuals were no different than the general population.
However, this led to the manufacturer voluntarily withdrawing the vaccine in 2002. The withdrawal of LYMErix from the market was not due to its efficacy but rather due to concerns about its safety (even though no direct link was established between the vaccine and the reported adverse events) and threats of potential lawsuits.
Since the withdrawal of LYMErix, there have been ongoing efforts to develop new and effective vaccines against Lyme disease. Several promising candidates are in clinical trials now.
The observation that a number of celebrities have been diagnosed with Lyme disease and have spoken about it publicly has garnered attention and led to discussions on this topic. Here are some factors that might explain this phenomenon:
Potential Over-Diagnosis and False Diagnosis: There’s been debate and controversy in the medical community about the diagnosis and treatment of “chronic Lyme disease” or persistent symptoms attributed to Lyme disease. Lyme disease can be challenging to diagnose due to non-specific symptoms, which can overlap with many other conditions. People, especially celebrities with extensive financial resources, may seek a variety of opinions to address symptoms they are experiencing.
Some of these opinions sought from practitioners that do not have infectious disease expertise, including naturopaths, homeopaths, chiropractors, or physicians who completed training in unrelated medical fields. These practitioners are not covered by insurance but are quite popular in the celebrity space, where unfortunate predatory practices can lead them to profit substantially from prescribing long-term and ineffective treatments when there may not even be clinical or epidemiological evidence of Lyme.
As a result, Lyme disease can be over-diagnosed by practitioners who are not qualified to do so and even self-diagnosed by celebrities or other individuals who fall prey to misconceptions shared by celebrities.
Increased Awareness: When celebrities disclose their health conditions, it attracts more public attention and media coverage than when non-celebrities make similar disclosures. This can lead to a perception that the condition is more widespread than reality, and may lead others to believe they are suffering from a similar condition.
Diagnostic Challenges: Lyme disease can be challenging to diagnose due to its non-specific symptoms, which can overlap with other conditions. People, including celebrities, might go through extensive medical evaluations to identify the root cause of their symptoms. In many cases, these individuals have not met the clinical or epidemiological criteria for a Lyme disease diagnosis or may not have had documented evidence of a Borrelia burgdorferi infection. Many practitioners who diagnose this use unproven tests that report false positives using non-blood bodily fluids and unreliable testing technologies, leading people to believe they have an infection when they do not.
While celebrities may have been led to believe that their symptoms are due to a persistent, low-level infection, there is no credible evidence to support this. Remember, there are a variety of other medical conditions that have similar symptoms to the more generic signs of Lyme disease, and it is important to seek an accurate diagnosis from a credible healthcare provider.
Public Advocacy: Celebrities often have platforms that allow them to raise awareness for particular issues, including health conditions. Some celebrities have chosen to use their platforms to raise awareness about Lyme disease (whether they truly had Lyme disease or not), which brings more public attention to the topic.
General Prevalence: Lyme disease is the most common vector-borne illness in the U.S., with tens of thousands of confirmed cases each year. Given its overall prevalence, it’s not entirely unexpected that a number of celebrities would be diagnosed with it. However, there are routine reports of celebrities who have stated they have contracted Lyme disease in areas around the world where Lyme does not exist (such as Australia), have no evidence of a tick bite or circumstances in which they might have been exposed to infected ticks, or have publicly stated they sought unproven diagnostics and treatments.
While celebrities’ experiences with Lyme disease can draw attention to the condition and its challenges, it also draws attention to the misinformation about Lyme disease. As such, it’s essential to base health decisions and understandings on legitimated scientific evidence and consultation with credible healthcare professionals.
Lyme disease, caused by certain species of bacteria of the Borrelia genus, is found in many parts of the world, but is absent in other parts. In order for Lyme disease to be present, both tick species that can carry and transmit the disease-causing bacteria and the disease-causing bacteria must exist.
Lyme disease is found in North America, most commonly reported in the northeastern, north-central, and Pacific coastal regions of the United States. Canada also has areas where Lyme disease is prevalent, especially in the southeastern provinces. In North America, Lyme disease is caused by Borrelia burgdorferi and transmitted by the black-legged or deer tick and the westen black-legged ticks.
Lyme disease is present in countries across Europe, from Scandinavia in the north to countries like France, Germany, and Poland in central Europe, to some parts of southern Europe. In Europe, Lyme disease is caused primarily by Borrelia afzelii, Borrelia garinii, and less commonly, Borrelia burgdorferi and Borrelia bavariensis. The tick species that transmit these bacteria in Europe include the castor bean tick (Ixodes ricinus) and the taiga tick (Ixodes persulcatus).
In Europe, Lyme disease is endemic from southern Scandinavia into the northern Mediterranean countries of Italy, Spain, Portugal, and Greece and east from the British Isles into central Russia. Incidence is highest in Central and Eastern European countries. European countries with highest reported prevalence of Lyme disease include Estonia, Lithuania, Slovenia, Switzerland, France, Poland, Finland, and Latvia. Countries with lowest prevalence include Belgium, Bulgaria, Croatia, UK, Scotland, Ireland, Hungary, Norway, Portugal, Serbia, Russia.
There are rare reports of Lyme disease in temperate regions of some countries in Asia. Infected ticks occur from western Russia through Mongolia, northeastern China, and Japan; however, human infection appears to be uncommon in some of these areas. In Asia, Lyme disease is caused primarily by Borrelia afzelii, Borrelia garinii, and less commonly, Borrelia burgdorferi and Borrelia bavariensis. The tick species present in this geography include the castor bean tick (Ixodes ricinus) and the taiga tick (Ixodes persulcatus).
There is no confirmed presence of Lyme disease in other parts of the world including Australia, South America, and African countries. There is no definitive evidence that Borrelia burgdorferi or similar species as well as species of ticks that transmit these bacteria are present in these countries.
Symptom Presentation: While children can exhibit the wide range of symptoms associated with Lyme disease, certain manifestations might be more prominent or more commonly recognized in children. For instance:
- Children might be more likely to present with joint complaints, especially knee arthritis.
- Facial nerve palsy (a drooping of one side of the face, often mistaken for Bell’s palsy) is a relatively common presentation in children with Lyme disease.
- Children might be less likely to report or be able to articulate certain symptoms, such as fatigue or cognitive changes, compared to adults.
Erythema Migrans (EM) Rash: This characteristic “bull’s-eye” rash is a common early symptom of Lyme disease. In children, this rash might be overlooked if it’s located in a less visible area, such as the scalp. Parents and caregivers are often the ones to spot this rash.
Behavioral and Cognitive Changes: Some children with Lyme disease may experience behavioral changes, difficulty in school, or cognitive disturbances. These might manifest as mood swings, irritability, changes in school performance, or difficulties with concentration and memory.
Diagnosis Challenges: Children might have difficulty articulating their symptoms or might describe them differently than adults would. This can pose challenges in obtaining a clear clinical picture. Moreover, since children are often active and might have various bumps and bruises from play, initial symptoms might be dismissed or attributed to other causes.
Treatment: Antibiotic treatment for children with Lyme disease is generally similar to that for adults, but the specific antibiotic and dosage might vary based on the child’s age and weight.
Prevention: Because children often spend time playing outdoors, especially in grassy or wooded areas, they might be at an increased risk of tick bites. Educating children about safe outdoor habits, performing regular tick checks, and using appropriate tick repellents can help reduce the risk.
As with adults, early detection and treatment are crucial for children with Lyme disease. If a parent or caregiver suspects a child might have been exposed to a tick bite or is showing symptoms consistent with Lyme disease, they should seek medical evaluation promptly.
There are several tests used to diagnose Lyme disease, but determining if the disease is “cured” or if the infection has been eradicated can be challenging for several reasons:
Testing Limitations: The most common tests for Lyme disease include the enzyme immunoassay (EIA) and the Western blot. These tests detect antibodies against Borrelia burgdorferi. However, antibodies can remain in the body long after the bacteria have been eradicated, meaning a test might remain positive even if the disease is effectively treated and infection is eliminated.
Persistence of Symptoms: About 10-20% of patients report symptoms after successful antibiotic treatment, a condition known as Post-Treatment Lyme Disease Syndrome (PTLDS). These symptoms do not necessarily indicate ongoing active infection. Instead, they might result from residual tissue damage or an inflammatory response from infection. No current test can differentiate between ongoing infection and PTLDS.
Clinical Assessment: Often, the determination of a “cure” is based on clinical assessment rather than a specific test. If a patient was symptomatic and then improves after treatment, and no new symptoms appear, the treatment is considered successful.
Potential for Re-Infection: Even after successful treatment of Lyme disease, individuals can be re-infected if bitten by another infected tick. A subsequent positive test might represent a new infection rather than a relapse of the original one.
A positive antibody test for Lyme disease indicates that your immune system has produced antibodies in response to Borrelia burgdorferi (or closely related species), the bacteria that cause Lyme disease. However, a positive antibody test by itself doesn’t necessarily confirm an active Lyme disease infection for a few reasons:
Persistence of Antibodies: Once produced, antibodies to Borrelia burgdorferi can remain in your system for years after the infection has been treated and cleared. Therefore, a person who was infected with Lyme disease in the past, even if it was successfully treated and the infection was eliminated, could still have a positive antibody test.
False Positives: Other infections or conditions can sometimes cause a false-positive result on Lyme disease antibody tests. This is one reason why the two-tiered testing approach is recommended for Lyme disease: first, an enzyme immunoassay (EIA), followed by a Western blot if the EIA is positive. This two-step process helps improve the accuracy of Lyme disease testing.
Clinical Context: A positive antibody test is most meaningful when considered in conjunction with clinical symptoms and a history of potential exposure to infected ticks. For example, a positive antibody test in someone with a characteristic erythema migrans rash (often described as a “bull’s-eye” rash) and a history of being in a Lyme-endemic area would be highly suggestive of Lyme disease.
If you have a positive antibody test for Lyme disease, it’s essential to consult with a healthcare provider to interpret the result in the context of your symptoms, history, and any other relevant factors. They can help determine whether you have an active infection, a past infection, or if further testing or evaluation is needed.
